As someone who has personally navigated the challenges of living with an ostomy, I know firsthand how daunting it can be to figure out the right ostomy diet after surgery. Several years ago, I underwent colon cancer surgery that resulted in a temporary ostomy. Although mine was not permanent, the experience left a lasting impact on me and sparked a deep interest in focusing on proper nutrition.

When I found out that I would be getting an ostomy, I (almost) instantly became obsessed with my soon-to-be diet and wanted to learn more about what I could and could not eat. Of course, I had a medical team to help guide me, but I always liked to learn as much as I could on my own. Especially when it comes to my nutrition. Because let's face it. Most doctors don't know that much about nutrition.
In this guide, I aim to provide clear, actionable advice on crafting an ostomy diet that supports your healing process. We'll explore everything from the gentle embrace of bland and low-fiber foods to the careful reintroduction of more complex fare, all informed by my own firsthand experience and the insights I've gained along the way.
Together, we'll delve into dietary transitions, strategies for handling common challenges, and the importance of seeking support and guidance from healthcare professionals and fellow ostomates. My goal is to empower you with the knowledge and tools you need to thrive with an ostomy, without overwhelming you with excessive details or pressuring you to use specific products.
So, let's embark on this journey together, one nourishing meal at a time.
This post is all about an "Ostomy Diet".
Please note that I am not a medical professional and this post contains general information that should not replace the advice of your doctor or nurse.
Key Takeaways
- A balanced ostomy diet, focusing on bland, low-fiber, and thoroughly cooked foods, aids in digestion and promotes healing post-surgery.
- Transitioning from a liquid (such as juices or smoothies) to a solid diet after ostomy surgery should be gradual, starting with basic liquids, moving on to soft foods, and carefully incorporating solid foods while monitoring the body’s reaction.
- Managing common dietary challenges like gas, diarrhea, and constipation is crucial, and seeking guidance from healthcare professionals, including dietitians and support groups, can provide valuable support and tailored advice for living with an ostomy.
Choosing the Right Foods for Your Ostomy Diet

Embarking on the road to recovery post-ostomy surgery begins with the foods you choose to eat. It’s not about restrictions; it’s about discovering what foods play well with your body to nurture healing. A diet tailored to your needs can be a game-changer, easing digestion and promoting restorative processes. Imagine your diet as the gentlest, most supportive friend, offering comfort when you need it most.
The selection of the right foods involves embracing bland, low-fiber, and cooked varieties that are kind to your digestive system. This means giving a warm welcome to foods that won’t overburden your healing bowels and bidding a temporary farewell to those that might.
It’s all about finding that golden balance to ensure a smooth transition back into your diet, where each meal brings peace of mind and a sense of well-being.
Let’s delve into the specifics, shall we?
1. Introducing Soft (and Bland) Foods

Transitioning to bland foods post-colostomy isn’t about dull flavors—it’s about giving your digestive system the break it deserves. Picture a comforting bowl of cooked cereal or a simple plate of pasta and eventually lean proteins; these are the foods that will guide you through recovery with ease. They are the unsung heroes in your colostomy diet, providing sustenance without the fanfare of spices and complexity.
Some examples of bland soft foods include:
- Mashed potatoes
- Yogurt
- Applesauce
- Scrambled eggs
- Cooked vegetables (no skins or seeds!)
- Soft fruits like bananas and avocados
- Creamy peanut butter
These foods are perfect for anyone transitioning from a liquid diet, as they are easy to chew and swallow, making them ideal for chewing food.
Soft foods such as refined grains, smooth proteins, and milk and dairy products not only nourish but also comfort your still-sensitive digestive system. They’re like a trusted guide, leading you through a landscape that’s slowly becoming more familiar. With each well-cooked vegetable and each piece of easily digestible fruit, you’re building strength and resilience, preparing for the day when your diet can expand to include certain foods even further, such as high fat foods, fried foods, and spicy foods, as you learn to digest food more efficiently.
2. Choose Low-Fiber Foods

Low-fiber foods are the cornerstones of early post-surgery nutrition, acting as the gentle guardians of your recovering digestive system. These foods come with an unspoken promise: to minimize digestive workload and prevent any blockages that could derail recovery.
It’s about choosing the right companions for your journey—foods without skins or seeds that can be digested without a fuss. To ensure a smooth recovery, it’s important to avoid high fiber foods and focus on their low fiber counterparts.
Some examples of low-fiber foods include:
- White bread
- White rice
- Pasta
- Cooked vegetables without skins
- Skinless chicken or turkey
- Fish
- Eggs
- Smooth nut butters
- Soft fruits without seeds
These foods will help support your recovery and ensure a smooth transition back to a regular diet.
3. Opt for Cooked Foods
As you navigate your post-ostomy diet, cooked foods emerge as a key component in promoting digestive comfort and ease. The process of cooking not only softens the fibers in food, making them more easily digestible, but also reduces the acidity and potential for stomach upset. Your recovering digestive system will appreciate the gentle nature of bland, cooked foods, which are less likely to cause irritation or discomfort compared to their fatty or spicy counterparts.
For those who have undergone a colostomy, opting for cooked foods over raw ones is especially important. Raw foods, while nutritious, can be more challenging for your body to break down and process effectively. By cooking your meals, you're essentially giving your digestive system a helping hand, allowing it to absorb the nutrients it needs without undue strain. So, whether it's a comforting bowl of soup or a plate of well-steamed vegetables, know that each cooked meal is a step towards nourishing your body in the most gentle and supportive way possible.
4. Starting with a Liquid Ostomy Diet

After surgery, your digestive system is like a newborn—delicate, sensitive, and adapting to a whole new world. The transition from a liquid diet to solid foods is KEY in this adaptation process. It’s similar to teaching a child to walk, taking it one step at a time, ensuring stability and confidence with each new food introduced.
Starting with a liquid diet is the first gentle step, a way to hydrate and nourish without overwhelming your digestive system. Plus, it gives your system the ability to easier absorb nutrients that might otherwise be lacking in this ostomy diet. It was 100% essential for me to getting the vitamins that I needed to feel whole again (that is, until my body was able to process more robust foods).
Let’s look at how to navigate this transition with care and precision.
Liquid Diet Recommendations
A sip of water, the warmth of broth, the quiver of plain gelatin—these are the humble beginnings of your post-surgery diet. The clear liquid diet is your body’s first encounter with nourishment after the operation, a gentle introduction to eating that supports your recovery. It’s a soothing interlude, providing essential hydration while your digestive system takes its first tentative steps towards healing.
During this phase, it’s important to embrace non-caffeinated and non-carbonated drinks, which offer hydration without the risk of discomfort or additional digestive stress. Some options to consider include:
- Water
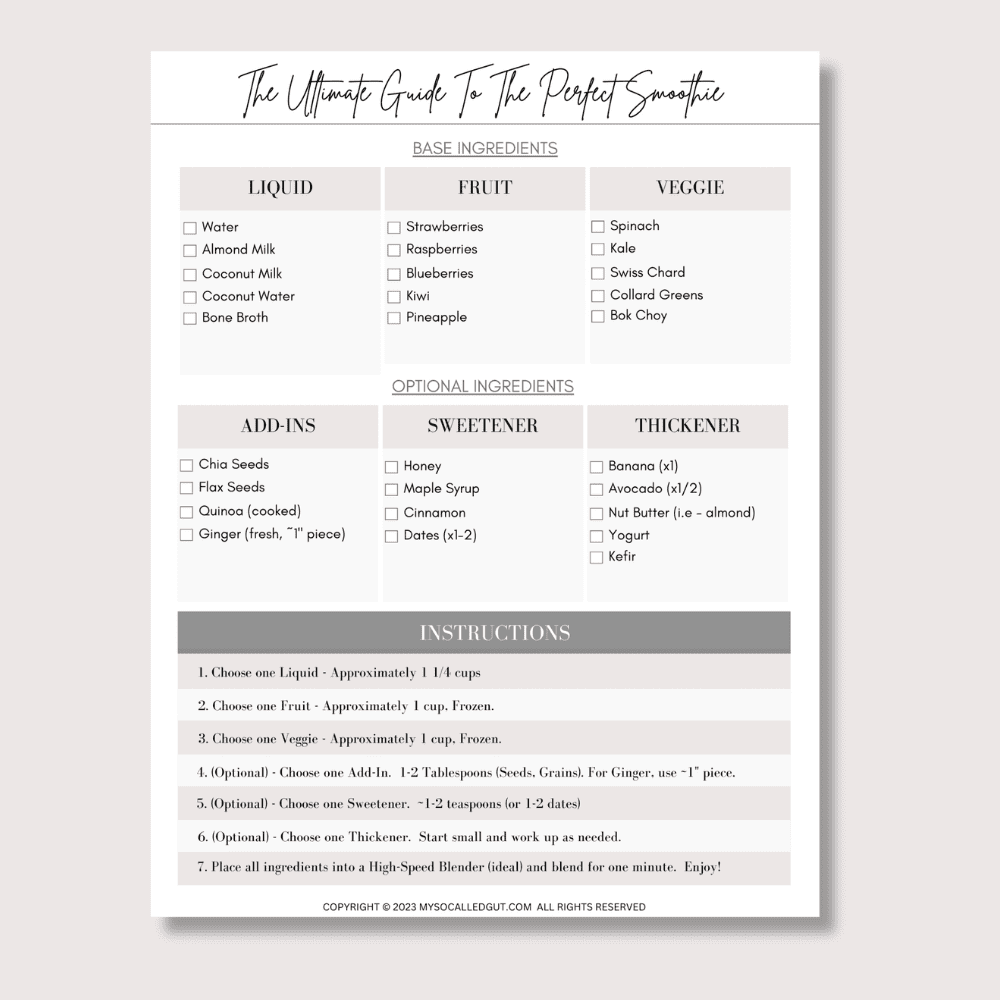
- Smoothies (well-blended, without seeds, skins, etc.)
- Juices (from fresh fruits and veggies)
- Herbal tea
- Coconut water
- Fruit-infused water
- Electrolyte-enhanced water
It’s worth noting that carbonated beverages are not recommended during this phase due to their potential to cause discomfort.
These drinks, including grape juice, can help replenish fluids and electrolytes gently and effectively.
This clear liquid diet is not just about sustenance; it’s about setting the stage for the more robust dietary acts to come.
5. Gradually Adding Solid Foods
When the time comes to introduce solid foods, it’s like adding color to a previously monochromatic diet. But this isn’t a process to be rushed; it’s a careful, considered integration of new textures and flavors. It’s about taking the time to chew thoroughly, to savor every bite, ensuring that each meal is a step forward, not backward.
Adding solid foods one at a time allows you to:
- Monitor your body’s reaction
- Understand which foods are friends and which are foes
- Have a personal journey where your body dictates the pace
- Practice patience for a smooth dietary transition
- Affirm your body’s ability to handle more
- Thrive under new conditions
Tips for Managing Common Dietary Challenges
Navigating dietary waters post-ostomy can sometimes feel like steering a ship through uncharted seas. Common challenges like gas, diarrhea, and constipation can arise, but with the right dietary guidelines, they can be skillfully managed. It’s about being the captain of your dietary ship, charting a course that avoids the turbulent waters of discomfort.
Meal planning, careful reintroduction of foods, and proper nutrient intake are your navigation tools, helping you steer clear of dietary pitfalls. It’s about knowing what to eat and when, ensuring that your meals are as balanced as they are beneficial. With thoughtful strategies, common dietary challenges can be transformed from daunting obstacles into manageable bumps on the road to recovery.
Gas and Odor Control
Gas and odor can be unwelcome guests in your post-ostomy life, but with the right strategies, you can show them the door. Limiting intake of gas-producing foods is like avoiding rough seas; it keeps your passage smooth and pleasant. Incorporating herbs and fermented dairy products is akin to a natural breeze, refreshing and odor-reducing.
Mindful eating habits, such as avoiding excess air ingestion, play a significant role in your quest for gas and odor control. It’s about fine-tuning your diet and lifestyle to ensure that your ostomy experience is as comfortable and dignified as possible. With these strategies, you can maintain a healthy diet and active life without the worry of unwelcome odors.
Diarrhea Management
Managing diarrhea is about finding the right balance in your diet, ensuring that your digestive system is neither overworked nor undernourished. Starchy foods and unsweetened applesauce are your allies, providing sustenance without exacerbating watery stools. Incorporating vegetables thickened stool applesauce into your diet can help achieve this balance. They’re like the steady hands that keep your ship stable amidst choppy waters.
Hydration is your lighthouse in the fog of diarrhea, guiding you to safety with plenty of fluids and electrolyte-rich foods. It’s about keeping your body replenished and resilient, ready to weather the storm. And with the right dietary adjustments, such as limiting alcohol and choosing lactose-free options, you can navigate the challenge of diarrhea with confidence and ease.
Constipation Prevention
Preventing constipation is about laying down the right dietary tracks for your digestive train to run smoothly. Hydration is the steam that keeps the engine going, with 8 to 10 cups of water a day ensuring that everything moves along as it should. It’s about creating a fluid rhythm that keeps your digestive tune harmonious.
Gradually introducing fiber and ensuring regular exercise are like the switches on your track, guiding your digestive journey in the right direction. Smaller, frequent meals are the steady beats that prevent your system from becoming overwhelmed. With these preventative strategies in place, constipation becomes a distant concern, allowing you to focus on the joy of your recovery journey.
Adapting to Life with an Ostomy Bag
Life with an ostomy bag is a new chapter, one where adapting and thriving are the central themes. It’s about learning to live with a new normal, finding ways to comfortably integrate your ostomy into your daily life. Whether it’s work, sports, or social engagements, you can navigate these activities with confidence and grace.
Adaptation is a continuous process, and here are some tips to help you along the way:
- Ensure a proper fit of your ostomy appliance
- Find the right clothes that make you feel confident
- Discover what works for you
- Embrace the support of others who have walked this path before
- Take it one day at a time and find new ways to make living with an ostomy bag a seamless part of your life.
Improving Food Tolerances
Improving food tolerances post-ostomy is akin to cultivating a garden; it requires patience, care, and a willingness to learn. Experimentation is your gardening tool, helping you discover which foods your body can embrace and which it might reject. It’s a journey of discovery, one that allows you to customize your diet to your body’s unique needs.
Introducing different foods one at a time is like planting seeds individually, nurturing each one to see how it grows. This careful approach allows you to understand your body’s responses, giving you the knowledge to create a diet that is as diverse as it is digestible. With time and attention, you’ll find that your food tolerances can blossom into a rich array of dietary options.
Seeking Professional Guidance and Support
No matter where you are on your ostomy journey, seeking professional guidance and support can illuminate your path like a guiding star. Healthcare providers, including ostomy doctors and nutritionists, are ready to offer you the tailored advice that can make a world of difference. They’re the allies who can help you tackle any challenge, from managing your diet to navigating work life with an ostomy.
But it’s not just about physical health—psychological well-being is also a critical piece of the puzzle. By connecting with professionals who understand the intricacies of life with an ostomy, you can gain not only practical advice but also emotional support. It’s about building a support system that nourishes both body and soul.
Consulting a Dietitian
When it comes to your diet after ostomy surgery, dietitians are the culinary architects who can help you construct a meal plan that’s both satisfying and suitable for your new digestive landscape. Their expertise is invaluable, offering personalized guidance that considers the unique nutritional needs dictated by the location of your stoma. Think of them as the chefs who tailor the menu to your specific dietary requirements.
Dietitians are an integral part of your healthcare team, providing vital education and support to help you manage nutrition-related ostomy complications. They’re the ones who help you turn dietary advice into delicious meals, ensuring that your plates are as nourishing as they are appetizing. With a dietitian’s guidance, you can confidently navigate your dietary journey, making each meal a step towards optimal health.
Connecting with Ostomy Support Groups
Embarking on the ostomy journey can feel isolating at times, but ostomy support groups are the communities where you can find camaraderie and understanding. Within these groups, you’re free to express your feelings, share your experiences, and ask questions that only fellow ostomates could truly understand. It’s like finding a safe harbor where you can anchor your concerns and receive guidance from those who’ve navigated similar waters.
Organizations like the UOAA and IOA not only provide support but also advocate for the ostomy community on a global scale. Additionally, online platforms such as the ConvaTec Great Comebacks Community offer a wealth of resources and a space for discussion, making support accessible from the comfort of your home. Whether in person or online, these support groups are the lifelines that can keep you afloat during challenging times and celebrate with you during your triumphs.
Summary
As someone who has been in your shoes, navigating the challenges of living with an ostomy, I know firsthand how overwhelming it can be to figure out the right ostomy diet after surgery.
Throughout this guide, my goal has been to share the insights I've gained from my own experience and provide you with clear, actionable advice on crafting an ostomy diet that supports your healing process. We've explored everything from the gentle comfort of bland, low-fiber foods to the careful reintroduction of more complex foods. I hope that by sharing my journey, you'll feel empowered to tackle the dietary transitions, common challenges, and emotional hurdles that come with adapting to life with an ostomy.
Remember, you're not alone in this. Seeking support and guidance from healthcare professionals and fellow ostomates can make all the difference. Don't hesitate to reach out, ask questions, and lean on the wealth of knowledge and compassion that exists within the ostomy community.
Embrace this journey, one nourishing meal at a time. Trust in your resilience, and know that with the right tools and mindset, you can thrive with an ostomy. I'm rooting for you every step of the way.
Frequently Asked Questions
What is the best diet after an ostomy?
After getting an ostomy, it's best to focus on a diet that includes refined grains like white bread and rice, low-fiber fruits and vegetables, and high-protein foods such as lean meats, eggs, low-fat dairy, and nut butters (smooth, non-chunky). These foods are generally easier to digest and can support wound healing during your recovery.
What foods should you avoid with an ostomy bag?
When you have an ostomy, it's important to avoid foods that may cause blockages or digestive discomfort. Some common foods to limit or avoid include high-fiber items like raw vegetables with skins or stalks, fruits with seeds or skins, whole grains, nuts, seeds, dried fruits, and coconut products, as these can be more difficult for your body to process and may lead to constipation or blockages.
How do you lose belly fat with an ostomy?
To lose belly fat with an ostomy, consider eating low fat products, such as low fat dairy and lean proteins, as well as steamed or boiled fruits and vegetables (with no skin), with a doctor's approval for exercise.
What are some bland foods recommended after ostomy surgery?
After ostomy surgery, it's recommended to stick to bland foods like cooked cereals, white bread, pasta, rice, to support digestion and healing. Avoid spicy, high-fiber, or gas-producing foods.


